Patient Safety Considerations
- All patients should have drug allergies identified prior to administration of pain medication
- Administer opioids with caution to patients with GCS less than 15, hypotension, identified medication allergy, hypoxia (oxygen saturation less than 90%) after maximal supplemental oxygen therapy, or signs of hypoventilation
- Use of splinting techniques and application of ice should be done to reduce the total amount of medication used to keep the patient comfortable
Notes/Educational Pearls
Key Considerations
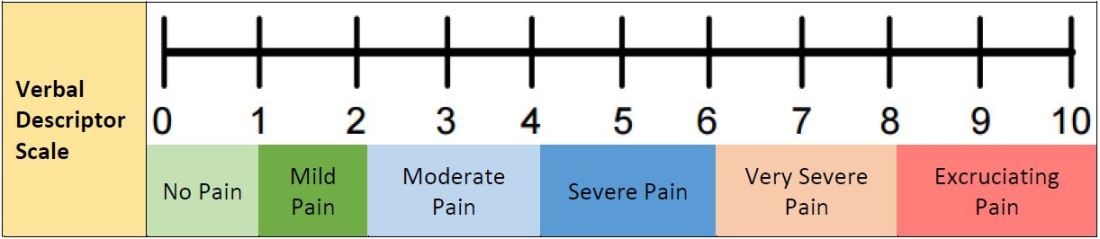
- Pain severity (0 – 10) should be recorded before and after analgesic medication administration and upon arrival at destination
- Patients with acute abdominal pain should receive analgesic interventions – Use of analgesics for acute abdominal pain does not mask clinical findings or delay diagnosis
- Opiates may cause a rise in intracranial pressure
Pertinent Assessment Findings
- Mental status (GCS and pain level)
- Respiratory system (tidal volume, chest rigidity)
- Gastrointestinal (assess for tenderness, rebound, guarding, and nausea)
Quality Improvement
Associated NEMSIS Protocol(s) (eProtocol.01)
- 9914071 – General-Pain Control
Key Documentation Elements
- Documentation of patient vital signs with pulse oximetry
- Acquisition of patient’s allergies prior to administration of medication
- Documentation of initial patient pain scale assessment
- Documentation of medication administration with correct dose
- Documentation of patient reassessment with repeat vital signs and patient pain scale assessment
Performance Measures
- The clinical efficacy of prehospital analgesia in terms of adequacy of dosing parameters
- EMS Compass® Measures (for additional information, see http://www.emscompass.org)
- PEDS-03: Documentation of estimated weight in kilograms. Frequency that weight or length-based estimate are documented in kilograms
- Trauma-01: Pain assessment of injured patients. Recognizing that pain is undertreated in injured patients, it is important to assess whether a patient is experiencing pain
- Trauma-02: Pain re-assessment of injured patients. Recognizing that pain is under-treated in injured patients, it is important to assess if a patient is experiencing pain
Universal Pain Assessment Tool


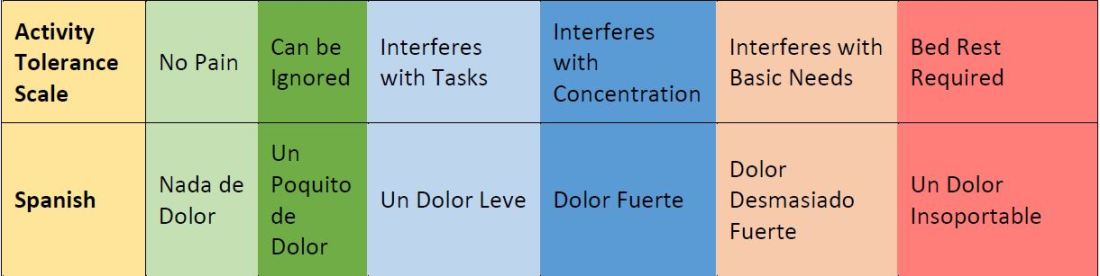

Faces, Legs, Activity, Cry, Consolablity (FLACC) Behavioral Scale
Appropriate age for use (per guideline): less than 4 years

Instructions:
- Patients who are awake: Observe for at least 1-2 minutes. Observe legs and body uncovered. Reposition patient or observe activity, assess body for tenseness and tone. Initiate consoling interventions if needed
- Patients who are asleep: Observe for at least 2 minutes or longer. Observe body and legs uncovered. If possible reposition the patient. Touch the body and assess for tenseness and tone.
- Face
- Score 0 point if patient has a relaxed face, eye contact and interest in surroundings
- Score 1 point if patient has a worried look to face, with eyebrows lowered, eyes partially closed, cheeks raised, mouth pursed
- Score 2 points if patient has deep furrows in the forehead, with closed eyes, open mouth and deep lines around nose/lips
- Legs
- Score 0 points if patient has usual tone and motion to limbs (legs and arms)
- Score 1 point if patient has increase tone, rigidity, tense, intermittent flexion/extension of limbs
- Score 2 points if patient has hyper tonicity, legs pulled tight, exaggerated flexion/extension of limbs, tremors
- Activity
- Score 0 points if patient moves easily and freely, normal activity/restrictions
- Score 1 point if patient shifts positions, hesitant to move, guarding, tense torso, pressure on body part
- Score 2 points if patient is in fixed position, rocking, side-to-side head movement, rubbing body part
- Cry
- Score 0 points if patient has no cry/moan awake or asleep
- Score 1 point if patient has occasional moans, cries, whimpers, sighs
- Score 2 points if patient has frequent/continuous moans, cries, grunts
- Consolablity
- Score 0 points if patient is calm and does not require consoling
- Score 1 point if patient responds to comfort by touch or talk in ½ – 1 minute
- Score 2 points if patient require constant consoling or is unconsoled after an extended time
Whenever feasible, behavioral measurement of pain should be used in conjunction with self-report.
When self-report is not possible, interpretation of pain behaviors and decision-making regarding treatment of pain requires careful consideration of the context in which the pain behaviors were observed.
Each category is scored on a 0-2 scale, which results in a total score of 0-10
Assessment of Behavioral Score:
- 0 = Relaxed and comfortable
- 1-3 = Mild discomfort
- 4-6 = Moderate pain
- 7-10 = Severe discomfort/pain
© 2002, The Regents of the University of Michigan. All Rights Reserved.
Source: The FLACC: A behavioral scale for scoring postoperative pain in young children, by S Merkel and others, 1997, Pediatr Nurse 23(3), p. 293–297.
References
- Attard AR, Corlett MJ, Kidner NJ, Leslie AP, Fraser IA. Safety of early pain relief for acute abdominal pain. BMJ. 1992;305(6853):554-6.
- Bieri D, Reeve R, Champion GD, Addico at L, Ziegler J. The Faces Pain Scale for the self-assessment of the severity of pain experienced by children: Development, initial validation and preliminary investigation for ratio scale properties. Pain 1990;41:139-150.
- Brewster GS, Herbert ME. Hoffman JR. Medical myth: analgesia should not be given to patients with acute abdominal pain because it obscures the diagnosis. West J Med. 2000;172(3):209-10.
- Prehospital use of Ketamine in Battlefield Analgesia 2012-13. Falls Church, VA: Defense Health Agency; March 8, 2012. Correspondence to Assistant Secretary of Defense (Health Affairs).
- De Nadal M, Munar F, Poca MA, Sahuquillo J, Garnacho A, Rosselló J. Cerebral hemodynamic effects of morphine and fentanyl in patients with severe head injury: absence of correlation to cerebral autoregulation. Anesthesia. 2000;92:1-11.
- Hicks CL, von Baeyer CL, Spafford P, van Korlaar I, Goodenough B. The Faces Pain Scale – Revised: Toward a common metric in pediatric pain measurement. Pain. 2001;93:173-83.
- Jennings PA, Cameron P, Bernard S. Ketamine as an analgesic in the pre-hospital setting: a systematic review. Acta Anaesthsiol Scand. 2011;55(6):638-43.
- LoVecchio F, Oster N, Sturmann K, Nelson LS, Flashner S, Finger R. The use of analgesics in patients with acute abdominal pain. J Emerg Med. 1997;15(6):775-9
- Manterola C, Astudillo P, Losada H, Pineda V, Sanhueza A, Vial M. Analgesia in patients with acute abdominal pain. Cochrane Database Syst Rev. 2007 Jul 18;(3)CD005660.
- Merkel S, e al. The FLACC: A behavioral scale for scoring postoperative pain in young children., Pediatr Nurse. 1997;23(3):293–7.
- Odhner M, Wegman D, Freeland N, Ingersoll G. Evaluation of a newly developed non-verbal pain scale (NVPS) for assessment of pain in sedated critically ill patients. Available at: http://www.aacn.org /AACN/NTIPoster.nsf/vwdoc/2004NTI Posters. Accessed July 18, 2017.
- Pace S, Burke TF. Intravenous morphine for early pain relief in patients with acute abdominal pain. Acad Emerg Med. 1996;3(12):1086-92.
- Porter K. Ketamine in prehospital care. Emerg Med J 2004;21:351-4.
- Ranji SR, Goldman LE, Simel DL, Shojania KG. Do opiates affect the clinical evaluation of patients with acute abdominal pain? JAMA. 2006;296(14):1764-74.
- Svenson JE, Abernathy MK. Ketamine for prehospital use: new look at an old drug. Am J Emerg Med. 2007;25:977-80.
- Vermuelen B, Morabia A, Unger PF, et al. Acute appendicitis: influence of early pain relief on the accuracy of clinical and US findings in the decision to operate – a randomized trial. Radiology. 1999;210(3):639-43.
- Wiel E, Zitouni D, Assez N, et al. Continuous infusion of ketamine for out-of-hospital isolated orthopedic injuries secondary to trauma: a randomized controlled trial. Prehosp Emerg Care. 2015;19(1);10-16.
- Wood PR. Ketamine: prehospital and in-hospital use. Trauma. 2003;5(2):137-40.