Aliases
Prone transport
Patient Care Goals
- Prioritize identification and treatment of immediately life-threatening medical conditions
- Monitor ventilation and oxygenation of the patient.
- Appropriate PPE (N95, goggles, gown, gloves) must be worn the entire transport
Patient Presentation
Inclusion Criteria
- Patients who have been diagnosed with COVID and require prone transport
Exclusion Criteria
- Patients who can be stabilized and transported Supine
- Patients who are in Cardiac Arrest
Patient Management
Assessment
- Confirm that the endotracheal tube is appropriately taped/controlled
- Make sure unstable patients who will be transported prone have cardiac pads placed on the patient
- Assess the perfusion and vital signs of the patient
- Ensure the patient is paralyzed for transport
Treatment and Interventions
- When connecting to our vent:
- Have the respiratory therapist perform an inspiratory hold on their vent
- While the patient is on the inspiratory hold, clamp the tube to prevent loss of PEEP
- Connect the tube the pre-programmed transport vent
- Unclamp the tube, and monitor for desaturations or patient distress
- Ensure the viral filter is place
- If the patient is not paralyzed/adequately sedated
- Please request paralysis and sedation prior to moving the patient
- If the patient cannot be paralyzed, please contact medical control
- If desaturation occurs
- Consider increasing the PEEP up to a max of 24
- If the patient is coughing/moving, increase sedation
- If hypotension occurs
- Consider push dose epinephrine
- Avoid fluid bolus as this can increase hypoxia
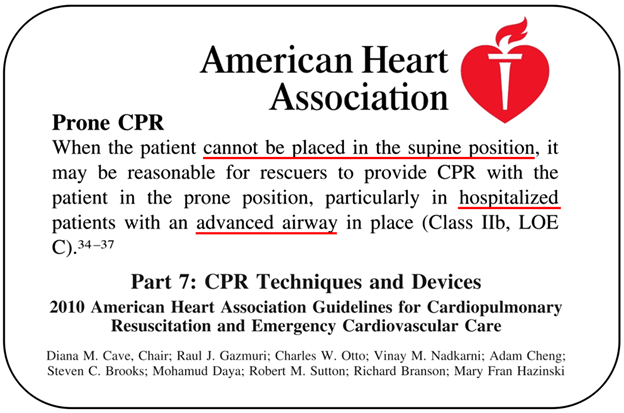
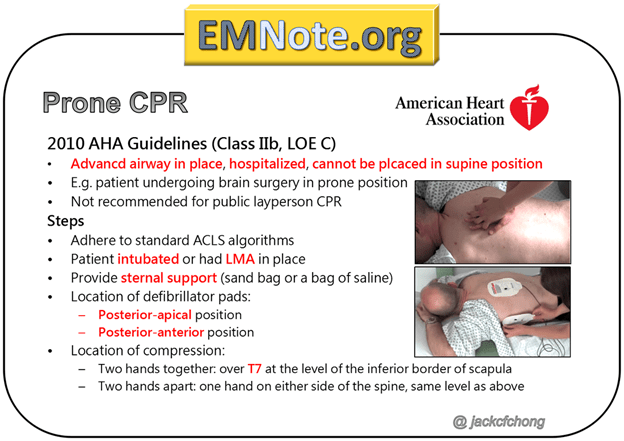
- If cardiac arrest occurs
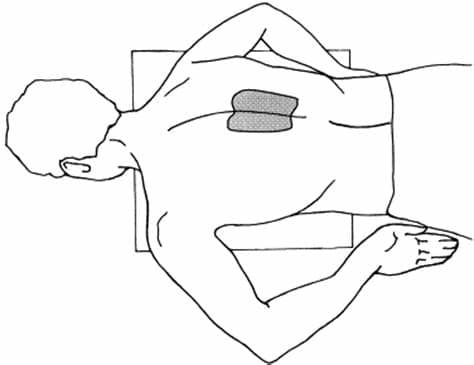
- Begin CPR while in a prone position
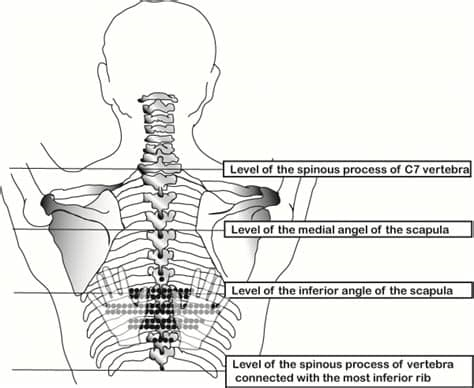
- Place hands on spine at the lower level of the scapula OR a hand on each side of the spaine at the lower aspect of the scapula. Perform CPR at 100 compressions per minute
- Begin CPR while in a prone position
- If you have more than 1 provider in the back, have one person disconnect the ET tube from the vent to provide bag-valve-mask ventilations on the highest PEEP setting
- Follow ACLS algorithm regarding medications and defibrillations
There is limited evidence for CPR in patients who are proned. Most literature is based on patients who have cardiac arrest during spinal surgery. Hypothetically, the AP compression is the same regardless if the patient is prone vs supine. The depth of chest compressions should be similar to the depth provided to a supine patient. Prone CPR is an acceptable option per the AHA. It is notable that patients who do have a cardiac arrest have a very high mortality rate, and a failure to get ROSC should not be perceived as a failure to provide appropriate care.
The largest risk to the patient during compressions is the loss of the endotracheal tube. Most of these patients will be transported with an additional nurse or medic. If CPR is initiated, the other team member must hold the tube in place during compressions.
Patients who are transported for COVID can be critically ill and may be on multiple medications. Below is a brief overview of some of the medications you may see during transport.
Propofol–
- Purpose: Used for sedation but lacks anesthetic (pain reduction) qualities. This will often be paired with fentanyl infusions.
- Side effects: bradycardia and hypotension are the most common side effects. It can also cause arrhythmias and slowed respiratory rate
- Other: It can be easily identified by the white (looks like you are infusing milk)
Ketamine–
- Purpose: Used for both sedation and pain. Has dissociative properties and hallucinogenic properties.
- Side effects: can cause tachycardia and hypertension.
- Other: Is often used as it has bronchodilation effects and limited respiratory depression
Dexmedetomidine/Precedex-
- Purpose: used for anxiolysis, sedation, and pain. It can be used to reduce agitation in patients who are not complete sedated (ie. to help with bipap)
- Side effects: At low concentrations it can cause hypotension, while at higher concentrations/rapid infusions it can cause hypertension. It can also be associated with bradycardia.
- Other: Can be associated with less delirium than other options. It is not really used for long-term sedation, but may be used for short-term sedation in an effort to reduce delirium
Rocuronium-
- Purpose: Paralytic. Has no sedation effects. The length of action of this medication is approximately 30-60 minutes
- Side effects: None
- Other: Can be reversed if needed. It is often used in severely ill patients to prevent patients from spending energy to breathe/prevent “fighting” the vent.
Vecuronium-
- Purpose: Paralytic. Has no sedation effects. Length of action is up to 60 minutes.
- Side effects: None
- Other: Can be reversed if needed. It is often used in severely ill patients to prevent patients from spending energy to breathe/prevent “fighting” the vent.
Dobutamine-
- Purpose: It is a pressor, used to raise blood pressure. It can significantly increase cardiac output and is used for cardiogenic shock.
- Side effects: Tachycardia, arrhythmias.
- Other:
Vasopressin-
- Purpose: It is used to augment pressors (rarely used alone). It can improve kidney function and reduce pulmonary hypertension.
- Side effects: Can cause fevers (rare), polyuria
- Other: This pressor is not titrated like other types of pressors. There are only three settings: high, low, and off.
Norepinephrine/Levophed-
- Purpose: Used to increased blood pressure, particularly in septic shock. Causes vasoconstriction.
- Side effects: Tachycardia
- Other:
Epinephrine-
- Purpose: Used as a pressor to increase blood pressure. Causes both vasoconstriction and increased cardiac output.
- Side effects: tachycardia
- Other:
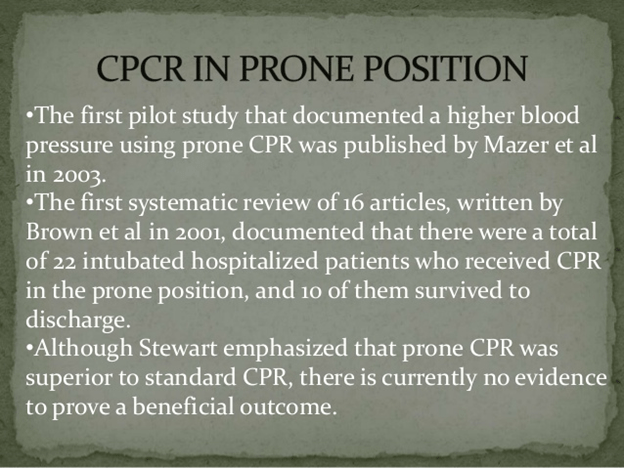
Reverse CPR: a pilot study of CPR in the prone position – PubMed (nih.gov)
ojanes2012050000114738359-1-130224074334-phpapp02-thumbnail-4.jpg (768×1043) (slidesharecdn.com)